|
ADDISON'S DISEASE

(HYPOADRENOCORTICISM)
THESE TERMS WILL BE USED INTERCHANGEABLY THROUGH THIS TEXT
|
ADRENAL HORMONES
The adrenal gland is so named because it is located just forward of the kidney ("renal" means kidney). The center of the gland is called the "medulla" and the outer area is called the "cortex." While both areas produce hormones, Addison's disease concerns the hormones produced by the cortex; these hormones are called "corticosteroids." Corticosteroids are the hormones that enable us to adapt physiologically to stress and, while our daily stresses are rarely life-threatening, our bodies still react to stress as if they were. When you (or your pet) experiences stress, the body prepares for "fight or flight."
We have corticosteroids for burning fat and sugar and corticosteroids for managing electrolytes all in preparation for "fight or flight."
The "Glucocorticoids" (such as cortisol and related synthetics, prednisone, dexamethasone and numerous others) act on the mechanics of sugar, fat, and protein metabolism. They gear the metabolism towards the preparation of burning (rather than storing) fuels so as to be ready for a "fight or flight" situation. After all, if one will be running or fighting for one's life, one will need readily available calories for success.
|
Kidneys are located at the
level of the lower back and
the adrenal glands (shown in yellow)
sit atop the kidneys.
(original graphic by marvistavet.com)
|
|
Cut surface of adrenal gland
(the outer layer, in yellow, is the cortex).
(original graphic by marvistavet.com)
|
The other corticosteroids are "Mineralocorticoids" and these are in charge of sodium and potassium balance. You may wonder what electrolytes have to do with fight or flight but it is important to remember that where there is sodium (salt), water soon follows. Conserving sodium will pull water from other tissues and bring it into the circulation ready to support blood pressure should a life-threatening bleed occur. The mineralocorticoid hormones instruct the kidney to retain sodium so that the circulatory changes of stress can be handled smoothly. As sodium is retained, potassium is lost in the exchange.
|
Corticosteroid hormones are needed to adapt to stressful situations and
without these hormones, even small stresses could lead to physiologic disaster.
HYPOADRENOCORTICISM (ADDISON'S DISEASE) IS A DEFICIENCY IN CORTICOSTEROID HORMONES
In animals with Addison's disease, there is a deficiency of the corticosteroid hormones. There are several reasons why this might happen: the adrenal gland might be damaged or drugs may be involved. We usually never find out what caused an individual patient's Addison's disease but the good news is that we don't need to know why it happened. Treatment is straight forward: we simply provide the hormones that the body is not making on its own.
|
CLINICAL SIGNS
Patients are usually young (age 4-5 years) dogs but any age dog can be affected. (This disease can occur in cats but it is very rare.) There is a genetic predisposition for Addison's disease in the Standard poodle and Bearded collie. Female dogs are affected twice as often as males.
|

Standard poodle
(Photocredit: Final4One via Wikimedia Commons)
|

Bearded collie
(Photocredit: MorgueFile.com)
|
At first signs are very vague - listlessness, possibly some vomiting or diarrhea. The pet just does not seem to feel right but not in an obvious way and may seem more or less normal most of the time as symptoms wax and wane with stress. This vague waxing and waning goes on and on with the dog never really getting fully sick but never staying well either. Eventually, the disease comes to a head in a phenomenon known as an "Addisonian crisis." The animal collapses in shock due to its inability to adapt to the caloric and circulatory requirements of stress. Blood sugar may drop dangerously low. Potassium levels soar and disrupt the heart rhythm because there is not enough conserved sodium to exchange for potassium. Heart rate slows, arrhythmias result. The patient may not survive this episode.
Approximately 30% of dogs with Addison's disease
are diagnosed at the time of an Addisonian crisis.
Approximately 90% of the adrenal cortex must be
non-functional to before clinical signs are observed.
MAKING THE DIAGNOSIS
Because of the numerous symptoms Addison’s disease can be present with, Addison’s disease has earned the medical nickname “The Great Imitator.” One would think that one could simply look for an increase in potassium and/or a drop in sodium on a basic laboratory blood panel, but it turns out spot checks of electrolyte values like this are not reliable enough for a diagnosis of Addison's disease.
Shock
Veterinarians are classically presented with a young animal in shock. There is usually no history of trauma or toxic exposure so general treatment for shock is initiated. This consists of rapid administration of fluids (usually lactated ringers solution which has little potassium and a moderate amount of sodium) plus some glucocorticoids. By coincidence, this also happens to be similar to the specific treatment for Addison's disease so that often the patient simply recovers without the veterinarian really knowing why.
Imitating Kidney Disease
The blood panel will come back showing elevations in the renal parameters (BUN and Creatinine) and thus with the elevated potassium is suggestive of acute renal failure, a condition with an extremely poor prognosis. The veterinarian may become suspicious of another diagnosis as the patient will respond well to fluid administration and most renal failure patients do not respond as well.
Low Blood Sugar
Addison’s disease may present in more unusual ways. Inability to maintain normal sugar levels (ultimately manifesting as a seizure disorder) may be strongly suggestive of an insulin-secreting pancreatic tumor but before a major abdominal surgery is planned, it is important to test for Addison’s disease.
Megaesophagus or Recurring GI Disease
In a similarly unexpected way, regurgitation of undigested food due to abnormal nerve function in the esophagus (a condition called “Megaesophagus”) can be caused ultimately by Addison’s disease. Megaesophagus has many causes but it is important not to forget Addison's disease. Of course, Addison's disease can also manifest with chronic waxing/waning diarrhea and/or poor appetite which would suggest a gastrointestinal problem such as inflammatory bowel disease. Before investing in the expense and potential anesthetic risk for endoscopy and intestinal biopsy, a screening test to rule out Addison's disease is prudent.
SORTING IT OUT WITH ACTH STIMULATION TEST
The only definitive test for Addison's disease is the ACTH stimulation test. The patient receives a dose of ACTH, the pituitary hormone responsible for the release of corticosteroids in times of stress. A normal animal will show an elevation in cortisol in response to ACTH while an Addisonian has no corticosteroids to respond with. This lack of response is diagnostic for Addison's disease; however, a false positive may be obtained if corticosteroids have been used in the treatment of the crisis prior to the test. Of all the commonly used corticosteroids, only dexamethasone does not interfere with the assay for cortisol; if any other steroid has been used, the test will not be valid for at least a couple of days.
TREATMENT
The most important aspect of treatment for hypoadrenocorticism is the replacement of the missing mineralocorticoids hormones. One way to do this is with oral fludrocortisone (Florinef®). Florinef is given usually twice a day at a dose determined by the patient's sodium and potassium blood tests. At first, these electrolytes are monitored weekly. When levels seem stable, these blood tests are repeated 2-4 times per year. Often with time, it will be found that the dose of Florinef needed to control the Addison's disease will increase. This is unfortunate as the medication is relatively expensive. Since Florinef has glucocorticoid activity as well as mineralocorticoid activity, it is usually not necessary to use additional medications for treatment. Using a compounding pharmacy may be helpful in managing the costs of this particular medication, especially in a larger dog.
|
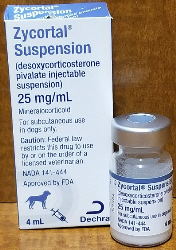
Another way to treat this condition is with an injectable medication called DOCP (brand names Percorten-V® and Zycortal®). This treatment is given approximately every 25 days. Electrolytes are measured prior to injections at first but testing can usually eventually be tapered to once or twice a year. There is some feeling among experts that DOCP produces better regulation of electrolytes than does oral Florinef. Dogs on DOCP, however, do require glucocorticoid supplementation (such as a low dose of prednisone).
|

(original graphic by marvistavet.com)
|
(original graphic by marvistavet.com)
|
WHAT IS "ATYPICAL ADDISON'S DISEASE?"
Most dogs become "Addisonian" when they lose the ability to produce mineralocorticoids and glucocorticoids both. They need both types of hormones replaced. It turns out that there is a subset of Addisonian dogs that are able to control their sodium/potassium imbalance through other hormones and only the glucocorticoids are in need of supplementation. These patients have what is called "Atypical Addison's disease." They can have all of the symptoms of typical Addison's disease as described above (chronic relapsing diarrhea/appetite loss, low blood sugar crisis etc.) but not the electrolyte shock crisis. Treatment consists of supplementation of glucocorticoid hormones, such as prednisone.
It was previously thought that these patients experienced only partial damage to their adrenal cortex and that is why they did not suffer full Addison's symptoms. More recently, however, it has been discovered that the atypical Addison's patients actually do have as much adrenal cortex damage as the typical Addison's patients; they have just found other ways to manage their sodium and potassium. Most atypical Addison's patients progress to the typical form which means they will eventually need more aggressive treatment with Florinef® tablets or Percorten® injections. The current recommendation is to monitor sodium and potassium levels every couple of months in atypical patients to watch for the switch to the typical (and more serious) form of Addison's disease.
WHAT IS SECONDARY ADDISON'S DISEASE
|
ACTH is the hormone made by the pituitary gland in times when glucocorticoid hormones are needed. The pituitary gland feels the glucocorticoid deficiency and sends a message to the adrenal gland telling it to produce and release more glucocorticoids. If the patient is being given glucocorticoids as a medical treatment, the pituitary will perceive that there are plenty of glucocorticoids in the body and will not release ACTH. The inner layers of adrenal cortex where glucocorticoids are made will atrophy. If medication is abruptly discontinued after long term use, the adrenal glands will be too atrophied to cover the body's demand for glucocorticoids. This creates a deficiency in glucocorticoids similar to atypical Addison's disease and is the reason why steroid hormones are typically tapered off rather than abruptly discontinued.
True atypical Addison's disease can be distinguished from overuse of medication by a plasma ACTH level (very high in atypical Addison's disease and very low with medication overuse). This is not simply of academic interest. The patient with secondary Addison's disease is never going to progress to typical Addison's disease and does not require long term periodic monitoring of electrolytes.
|
 Secondary Addison's disease usually from Secondary Addison's disease usually from
abrupt withdrawal of corticosteroid medication
(Photocredit: Morguefile.com) |
Extended corticosteroid use is not the only way to get secondary Addison's disease. Some dogs have pituitary glands that naturally secrete inadequate ACTH. ACTH is the hormone that tells the adrenal gland to produce and release its glucocorticoids. The pituitary may be diseased and unable to produce ACTH. When a patient appears to have the atypical form of Addison's disease, an ACTH level may be recommended to distinguish atypical from secondary Addison's disease.
WHAT IS "PACIFIC RIMISM"?
Dog breeds originating in the Pacific Rim, such as the Akita and Shiba inu, commonly have elevated potassium levels on blood tests. This can be very confusing when a patient has symptoms that suggest Addison's disease. These patients will have normal ACTH Stimulation test results if they do not have Addison's disease.
|
WHIPWORM INFECTION?
Whipworm infection has been known to create a syndrome nearly identical to Addisonian crisis, complete with abnormal sodium and potassium values. These patients will have normal ACTH stimulation tests but because whipworms only periodically shed eggs, fecal testing may not detect whipworm infection. If there is any question about whipworm infection, treatment should be instituted. See details on whipworm infection.
|
Adult Whipworm
(Photocredit: Alan R. Walker via Wikimedia)
|
Newsgroups for owners of pets with Addison’s disease are available. Here are some resources. Click to subscribe:
http://www.addisondogs.com/
https://canineaddisons.org
http://canineaddisonsinfo.com/Support.html

Page last updated: 1/13/2023
|